-
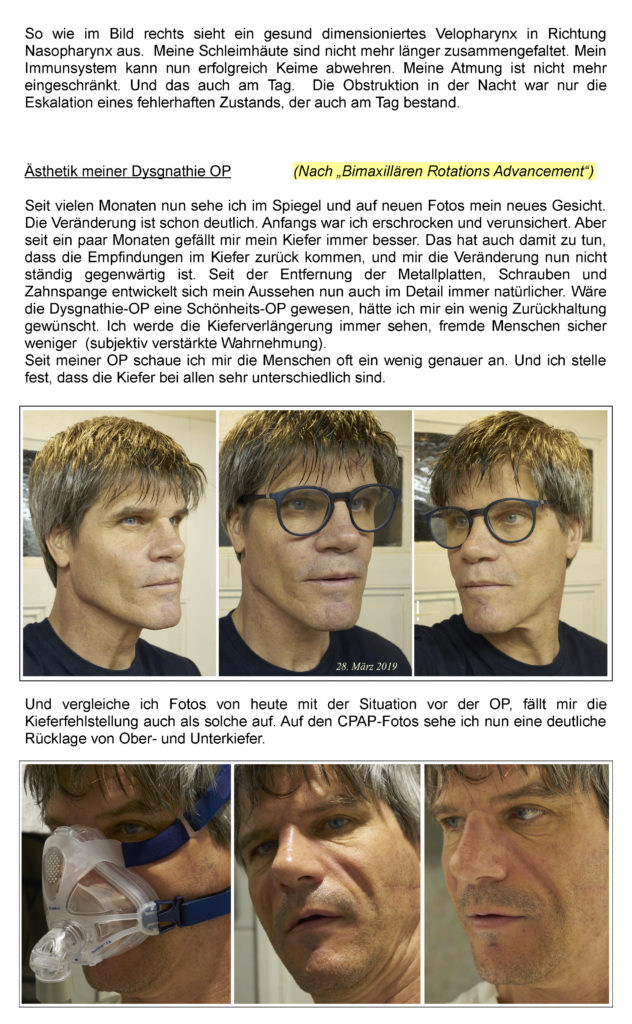
Before sleep apnea surgery
Before sleep apnea surgery
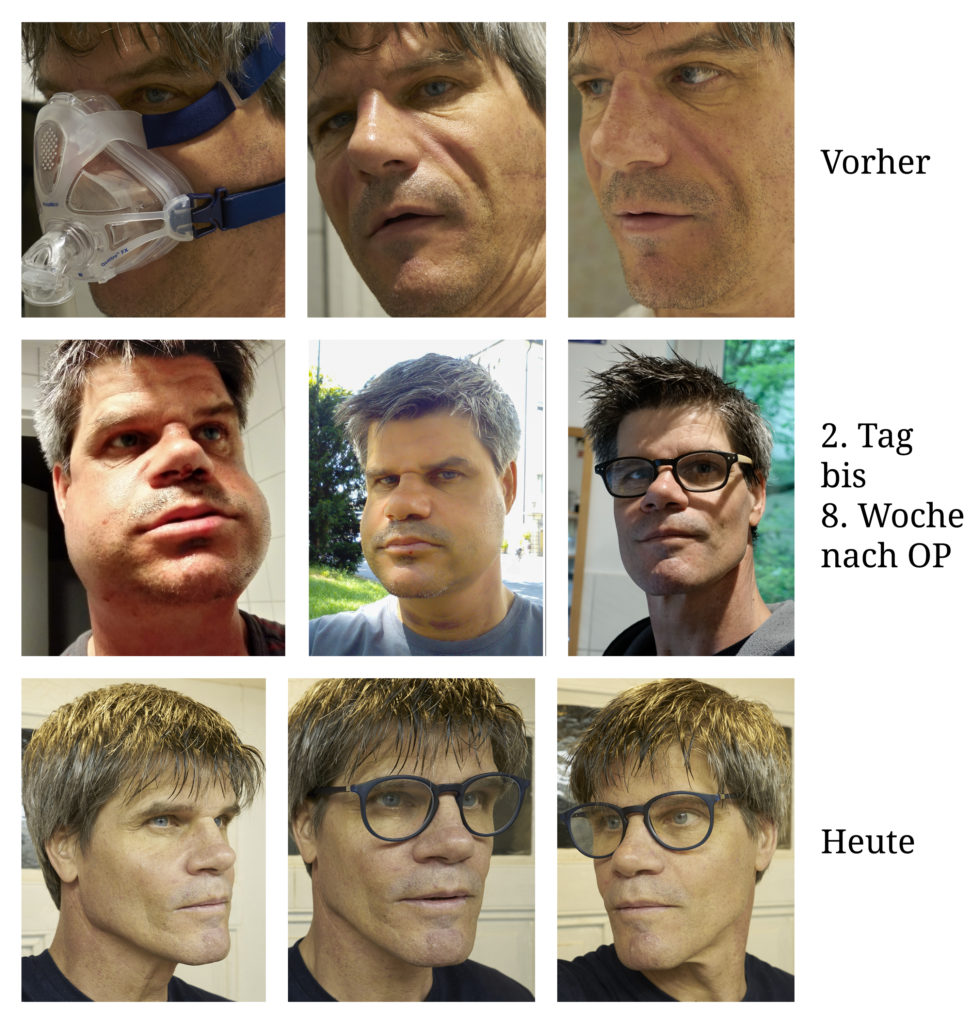
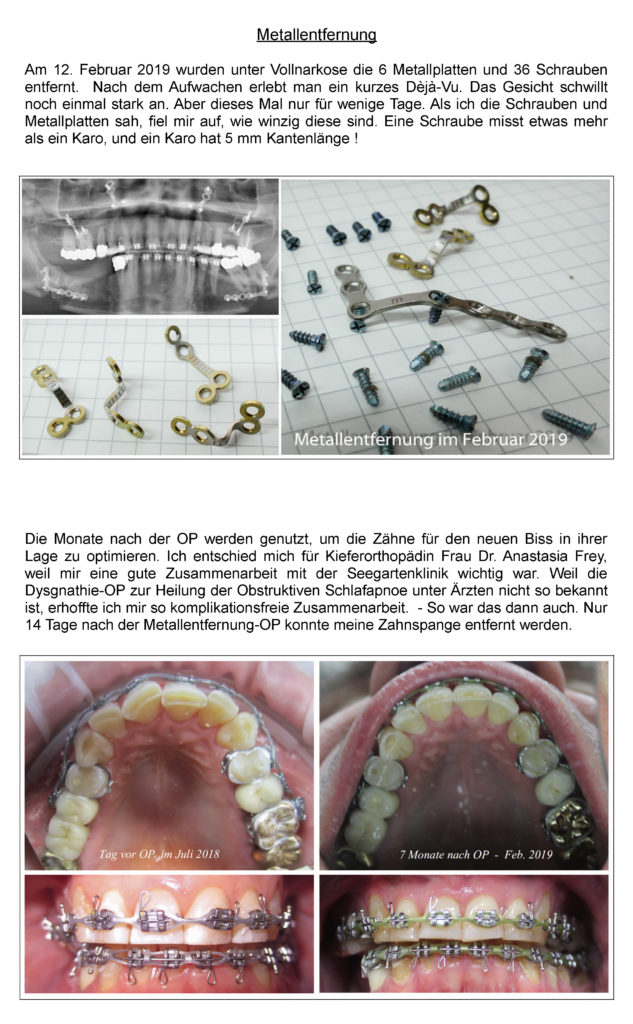
Today is March 1, 2019, and I am doing well. My surgery was on July 11, 2017, and I am glad I decided to have sleep apnea surgery at the Seagarden Clinic. I have already been able to sleep through the night for many months. Falling asleep happens quickly and without heart palpitations. In the years before the operation, my pulse increased after going to bed to the point of heart rhythm disorders, because my breathing was considerably impeded due to narrowed airways. Each breath was limited in flow by 50%. Always shortly before falling asleep I would startle. The heartbeat was elevated and only hesitantly returned to normal. Falling asleep was thus almost impossible. But because everyone has to sleep at some point, I also fell asleep after hours, only to be brought out of my sleep rhythm 153 times by the body's own wake-up reactions of the brain (CO2 increase). Restful sleep is thus impossible. In the morning I was awake only very hesitantly or dozed off without really regaining consciousness. First polygraphy (PG) in May 2017.
-
Cured from sleep apnea
Cured from sleep apnea
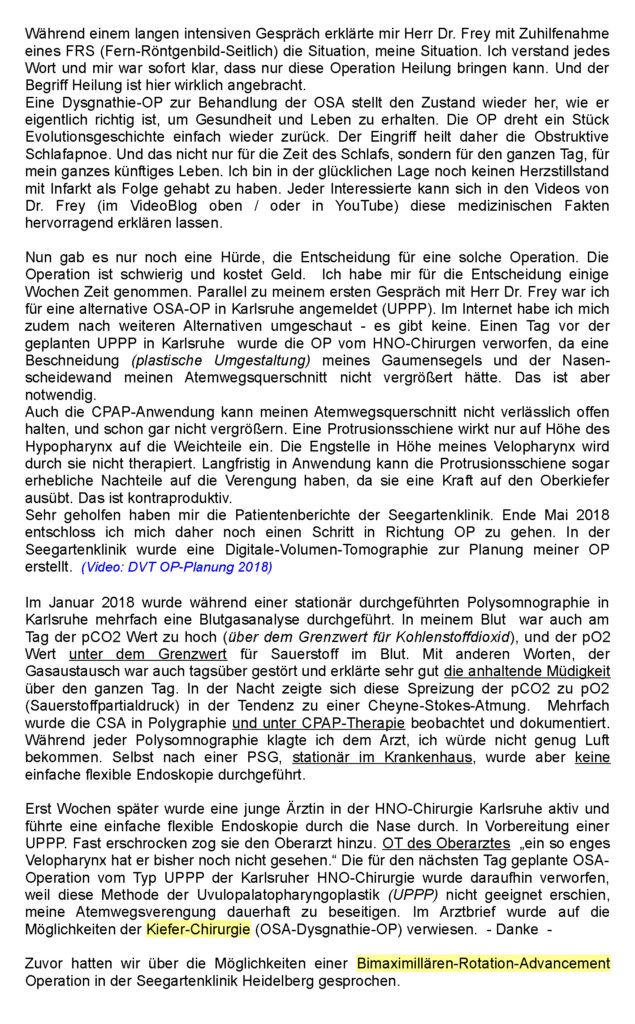
Today my sleep is restful and I dream a lot and coherently again. The hypopneas and apneas have decreased to zero. The snoring has also completely disappeared. This was not the case before the surgery and also under CPAP therapy. My daytime performance has increased significantly. In the 9th post-operative week, I started cycling and swimming again. During swimming, the improvement is evident from the first meter. I immediately swim 3 times the distance compared to before surgery. When swimming, the body is deep in the water, and breathing must now also work against the water pressure when inhaling. Due to the expansion of my airways by 250% in cross-section (at the narrowest point), there is now no resistance when breathing in and out. The air just flows in and out. The feeling of going under is gone.
But I also feel the improvement in everyday life from the first postoperative day. Already 14 days after the surgery I could walk the way from Heidelberg main station to the Seegartenklinik with my mouth closed without feeling shortness of breath. My breathing returned to normal. Until before the surgery, I had to breathe through my mouth at the slightest effort, lifting it up, because that was the only way I could get enough air.
-
The causes of my sleep apnea
The causes of my sleep apnea
I have been a non-smoker and non-drinker since I was born in 1965. Currently 53 years old. With a height of 185 cm and 77 kg weight a BMI of 22.5 BMI calculator on the Internet: Great! Your weight is healthy. With a balanced diet and regular exercise, it will stay that way in the long run.
An initial polygraph in 2017 showed poor sleep quality, many awakenings, central and obstructive apneas, hypopneas, and episodes of Cheyne-Stokes breathing. A 2018 polysomnography (sleep lab) identified obstructive sleep apnea syndrome with an AHI of 18.5. If obesity is a big factor in a high AHI, how should an AHI of 18.5 be assessed with a BMI of 22.5? Well, I can't reduce my weight to improve my situation, so there must be another reason for the obstruction.
-
The sleep apnea surgery
The sleep apnea surgery
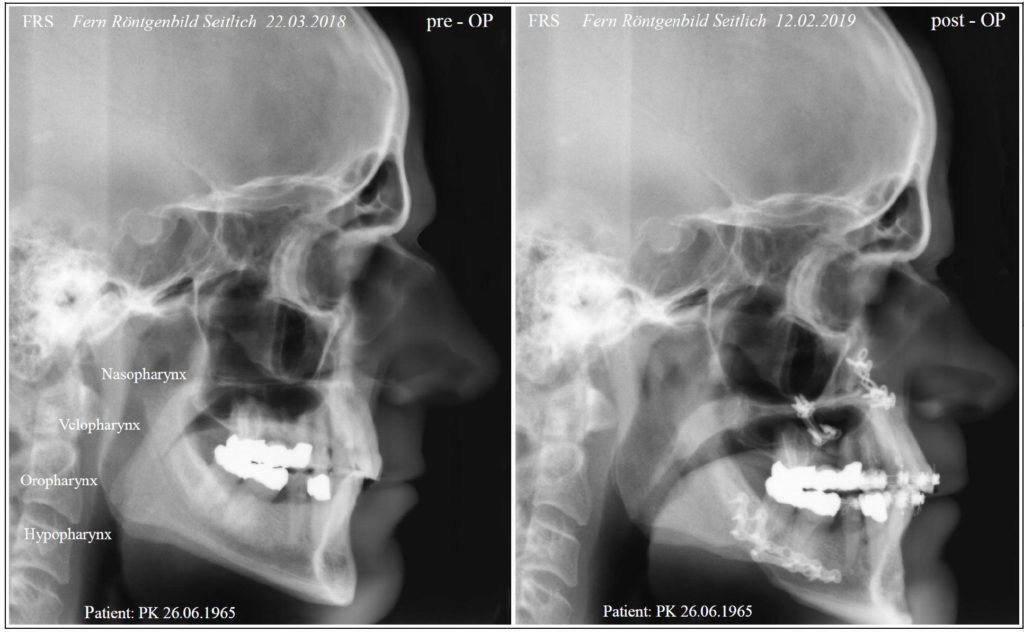
During a long intensive conversation, Dr. Frey explained to me the situation, my situation, with the help of a FRS (Fern-Röntgenbild-Seitlich). I understood every word and it was immediately clear to me that only this operation could bring healing. And the term cure is really appropriate here.
Jaw surgery to treat OSA restores the condition to what is actually right for health and life. The surgery simply turns back a piece of evolutionary history. Therefore, the surgery cures obstructive sleep apnea. And not only for the time of sleep, but for the whole day, for my whole future life. I am in the fortunate position of not having had a cardiac arrest with infarction as a result. Anyone interested can get an excellent explanation of these medical facts in Dr. Frey's videos (in the VideoBlog above / or in YouTube).
-
Decision for sleep apnea surgery
Decision for sleep apnea surgery
Now there was only one hurdle, the decision for such an operation. The operation is difficult and costs money. I took a few weeks to make the decision. Parallel to my first conversation with Dr. Frey, I was registered for an alternative OSA surgery in Karlsruhe (UPPP). I also looked around on the Internet for other alternatives - there were none. One day before the scheduled UPPP in Karlsruhe, the ENT surgeon discarded the surgery because a circumcision (plastic reshaping) of my soft palate and nasal septum would not have increased my airway cross-section. However, this is necessary.
Even CPAP application cannot reliably keep my airway cross-section open, and certainly not enlarge it. A protrusion splint only acts on the soft tissues at the level of the hypopharynx. It does not treat the constriction at the level of my velopharynx. In the long term, the protrusion splint can even have considerable disadvantages on the constriction because it exerts a force on the upper jaw. This is counterproductive.
I was very helped by the patient reports from the Seegartenklinik. At the end of May 2018, I therefore decided to take another step towards surgery. At the Seegartenklinik, a digital volume tomography was made to plan my surgery.
-
Recommendation for sleep apnea surgery by Klinikum Karlsruhe
Recommendation for sleep apnea surgery by Klinikum Karlsruhe
In January 2018, during an inpatient polysomnography in Karlsruhe, a blood gas analysis was performed several times. In my blood, even during the day, the pCO2 value was too high(above the limit for carbon dioxide), and the pO2 value was below the limit for oxygen in the blood. In other words, the gas exchange was also disturbed during the day and explained very well the persistent fatigue throughout the day. At night, this spread of pCO2 to pO2 (partial pressure of oxygen) showed a tendency toward Cheyne-Stokes respiration. On several occasions, CSA was observed and documented in polygraphy and under CPAP therapy. During each polysomnography, I complained to the doctor that I was not getting enough air. However, even after a PSG, inpatient in the hospital, a simple flexible endoscopy was not performed.
It was not until weeks later that a young female physician in the ENT surgery department in Karlsruhe became active and performed a simple flexible endoscopy through the nose. In preparation for a UPPP. Almost startled, she called in the senior physician. OT of the senior physician " he has not seen such a narrow velopharynx before." The UPPP type OSA surgery planned for the next day by Karlsruhe ENT surgery was then discarded because this method of uvulopalatopharyngoplasty (UPPP) did not seem suitable to permanently eliminate my airway narrowing. The doctor's letter referred to the possibilities of jaw surgery (OSA dysgnathia surgery). - Thank you -
-
Endoscopy of the respiratory tract
Endoscopy of the respiratory tract
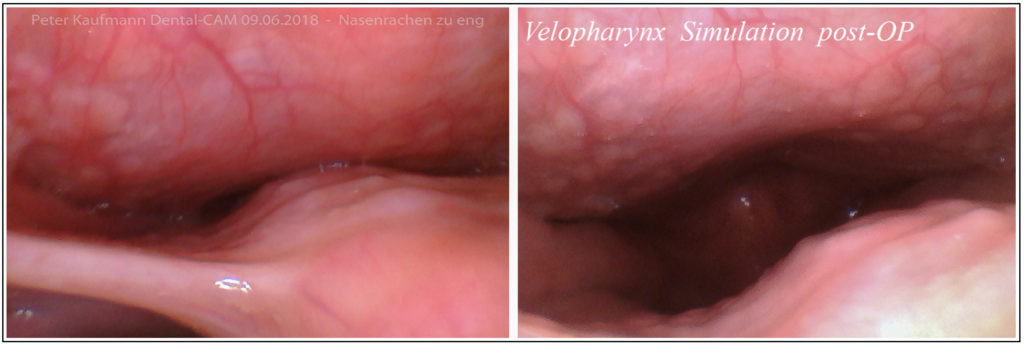
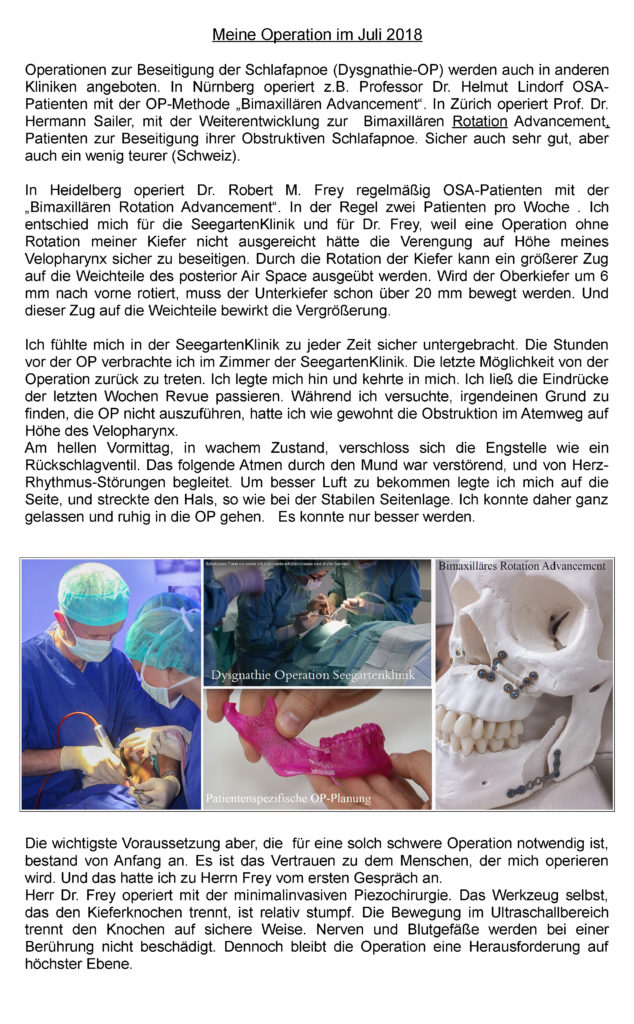
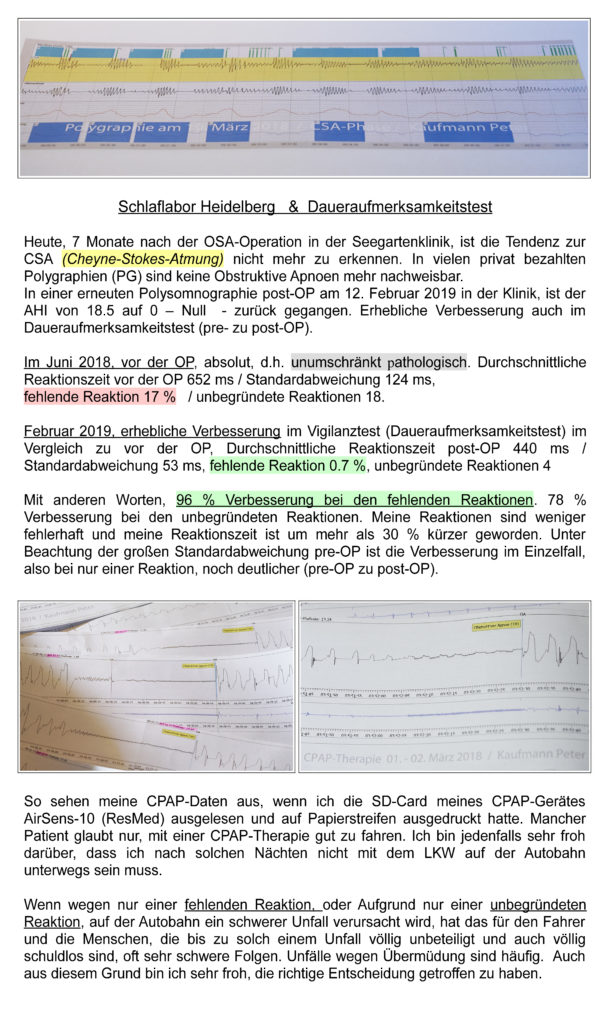
Both photos show my velopharynx. The mini-camera looks upward from the tongue into the nasopharynx. The left photo shows the tight permanent condition with the soft palate relaxed. The photo on the right shows a provoked openness of my velopharynx. I cannot maintain this state permanently. This open state can only be provoked by strong and fast exhalation with an open mouth.
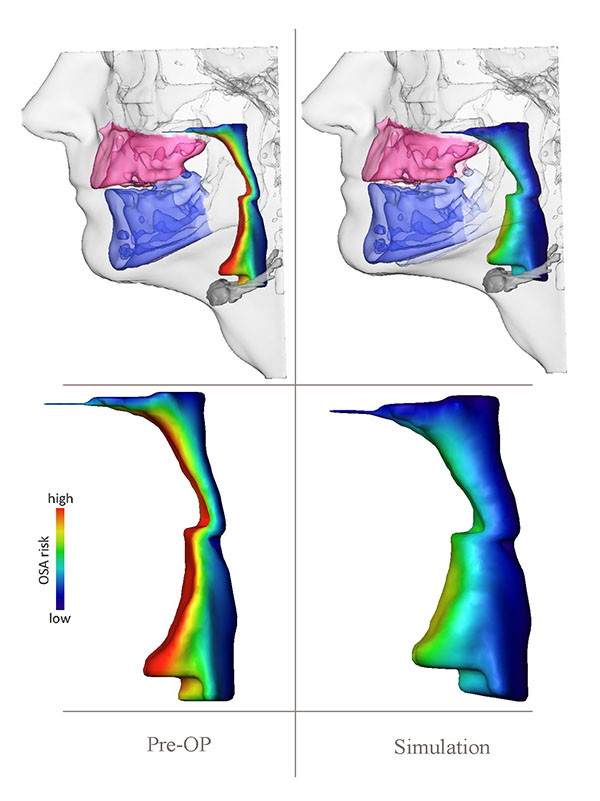
As shown in the photo on the right, it will hopefully look like this after the pre-displacement incl. a rotation of my upper jaw (bimaxillary rotation advancement). Hence the marking with simulation post-op. A simple advancement of only a few mm without rotation will not be sufficient to enlarge my velopharynx. This is due to the inertia with which the soft tissues can follow a forward displacement of the maxilla and mandible.
Both photos were taken in the sitting position. During the night in supine position, the constriction (left picture) closes like a check valve and exhalation is not possible. The CPAP therapy already prescribed in January 2018 could not satisfactorily prevent the apneas, hypopneas and flow limitations. Hourly, these even increased. At times, I had an apnea index of 30 under CPAP therapy for the duration of 45 minutes. With the hypopneas, an AHI of 45. In absolute terms, I spent 8 minutes in apnea during 45 minutes of CPAP therapy. The longest apnea 38 seconds.
Statistics are wonderful, but relative. The CPAP documented an AHI of 12 in the morning. After getting up, I felt exhausted, tired and listless. Despite CPAP therapy. However, the analysis of the CPAP data also showed that flow limitations and hypopneas that individually last less than 10 seconds but together extend over hours, or precede apneas, are not recorded in the AH index. But a sleep physician who loves CPAP does not look at my data in detail! He trusts his statistics. - Statistically, I slept relatively well with CPAP, but actually rather poorly. -
Recommendation of the Clinical Sleep Laboratory Karlsruhe
Recommendation of the Clinical Sleep Laboratory Karlsruhe
After the ENT surgery Karlsruhe, the senior physician of the clinical sleep laboratory Karlsruhe now also wrote in his doctor's letter about the CPAP therapy and its failure a recommendation for an oral surgery for dysgnathia.
"Sleep disturbed with increased arousal index of 35 per hour. CPAP increase due to relevant flow limitation and obstructive hypopneas was unsuccessful. A planned ENT surgery in Karlsruhe was again rejected. During a jaw surgery examination, imaging (digital volume tomography) showed a narrowing of the retropalatal space. It is possible that an oral surgical intervention can improve the nocturnal breathing situation. Yours sincerely" / gez. Senior physician (June 2018).
-
Bimaxillary Rotation Advancement
Bimaxillary Rotation Advancement
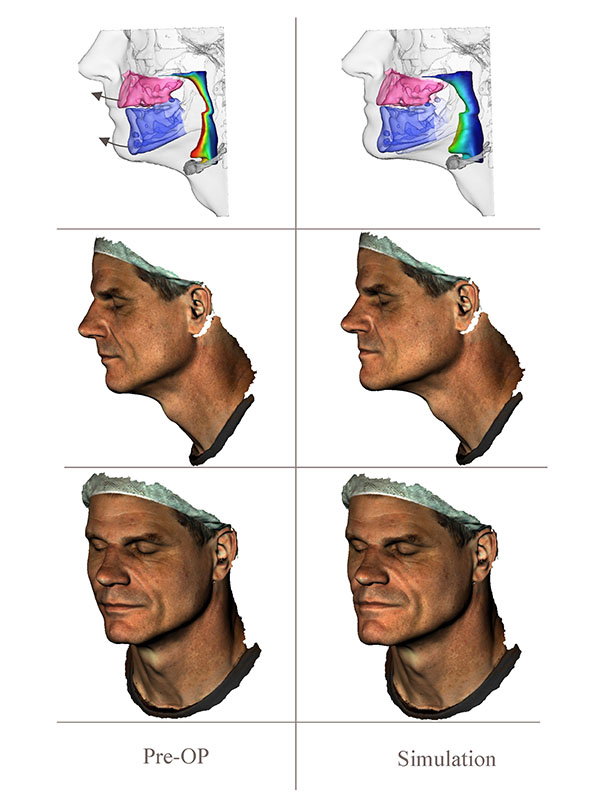
Previously, we had talked about the possibilities of bimaxillary rotational advancement surgery at the Seegartenklinik in Heidelberg. Bimaxillary because both jaws are moved in position. Advancement stands for advancing, improvement, further development. However, the decisive factor is the rotation of the jaws. Only by a rotation around a pivot point, which is very far in front, additional space is created in all 4 planes and the bite can be kept largely unchanged, or corrected with if necessary. Simply moving the jaws forward would not have been sufficient in my case. The Bimaxillary Rotation Advancement impressively eliminated the narrowing of my posterior air space from the nasopharynx - velopharynx - oropharynx down to the hypopharynx.

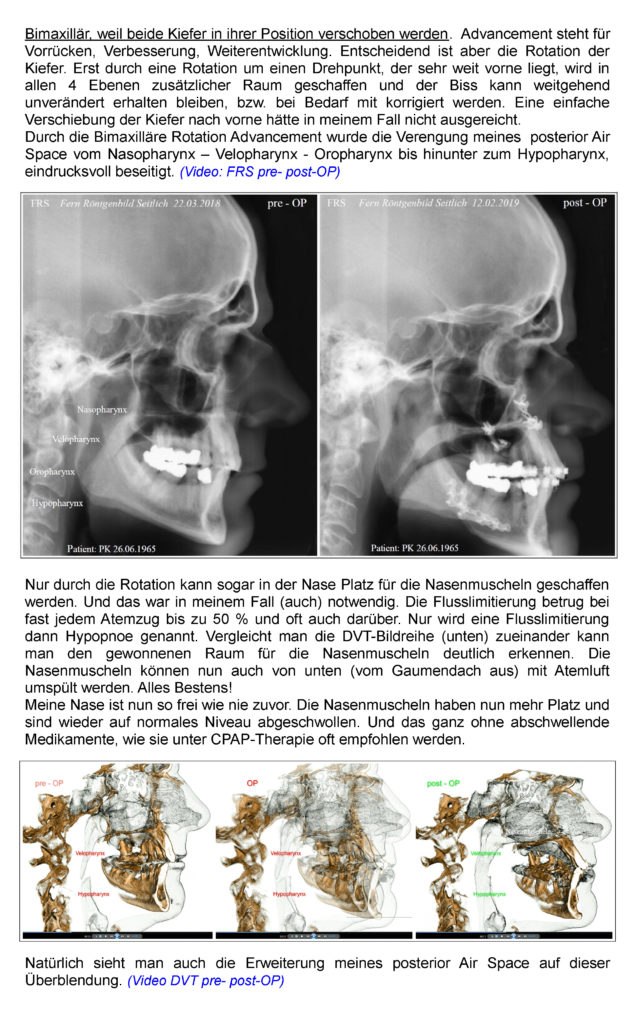



3D planning